NSCLC Non-Small-Cell Lung Cancer Pfizer Special Covid19 Jab Trial C4591024
Why did Pfizer have a special interest in the effects of their Jabs on NSCLC patients? Endotoxin is a prime suspect.
The recent passing of Jab pusher Susan Wojcicki was caused by Non-Small-Cell Lung Cancer (NSCLC).
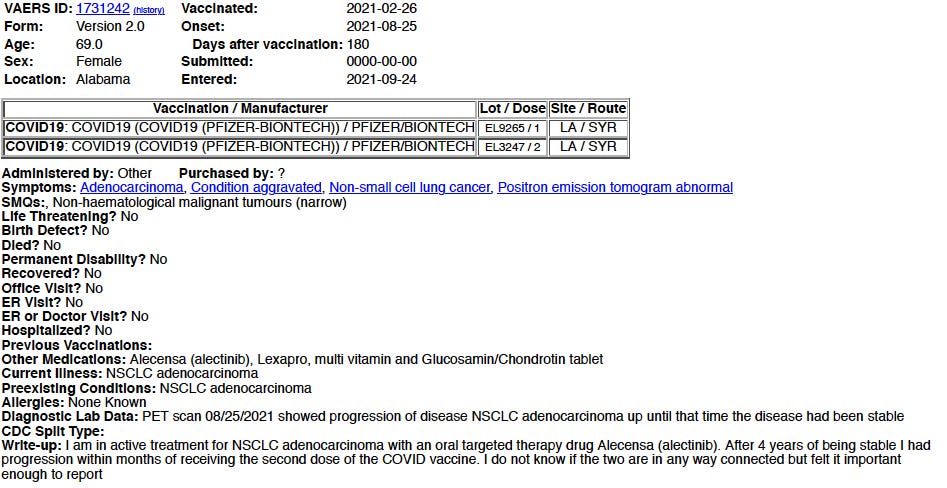
Searching VAERS we find case reports mentioning Turbo Cancer like this one lodged by a 69-year-old lady in Alabama who suffered progression of her previously stable NSCLC.
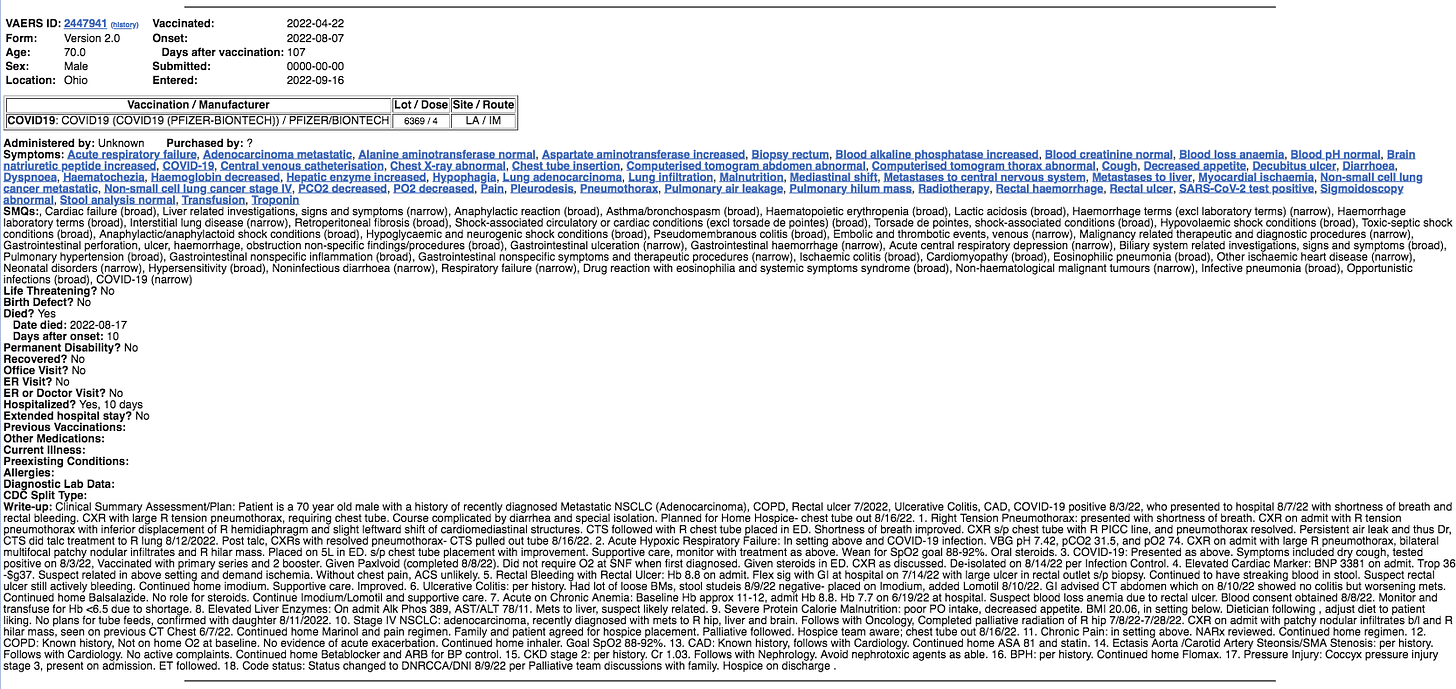
Pfizer Death from Sudden Onset NSCLC
A 70-year-old man died from NSCLC that moved to his hip, liver and brain.
Apparently his 4th Jab. His Lot Number 6369 could match 3 known Pfizer Batches.
Covid19 Jab Trial C4591024
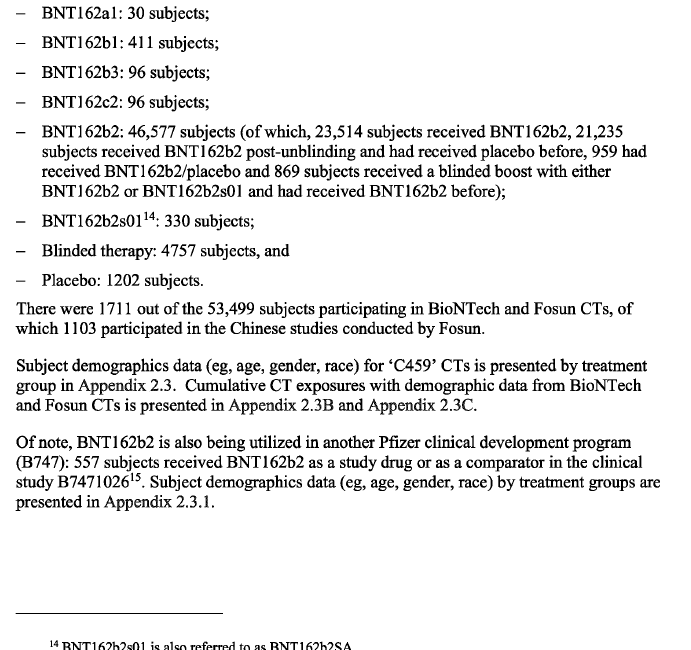
In an early article I reported that BioNTech and Pfizer conducted a special trial that included immunocompromised patients.1 There was just one patient with NSCLC.
This American Indian or Alaska Native male patient was aged 18 or over and took 3 jabs before withdrawing after the NSCLC had metastasized to his Bone.2 This patient was also classified as Hispanic/Latino.
After Dose 1 he suffered Diarrhea, Fatigue, New or worsened muscle pain;
After Jab 2 he suffered Diarrhea, Fatigue, Headache.
It is not clear what happend after his 3rd dose apart from the movement of his lung cancer to bone. That is usually fatal.
Pfizer Main Trial Unblinding NSCLC case
During its main trial a man who was initially in the Placebo Arm and then received Pfizer BNT162b jab and suffered Non-Small Cell Lung Cancer (NSCLC stage III) 31 days after his second jab.3
Endotoxin and NSCLC
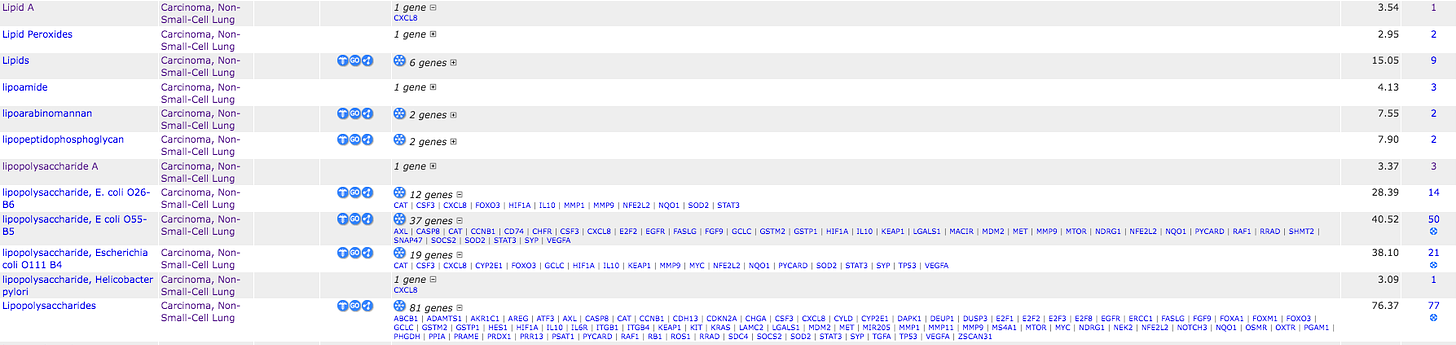
There is a vast literature on NSCLC linked to Endotoxin listed on the US Government Comparative Toxicogenomics Database (CTD) linked to dysregulation of over 80 genes.
Click to expand.
Searching PubMed for NSCLC returns 100,633 peer-reviewed papers.
Refining with Lipopolysaccharide gives 77 results.
Refining with LPS gives 76 results.
Refining with Endotoxin gives 35 results.
A very useful 2012 paper that is free to read reported Endotoxin induced cancer proliferation.4
Lung cancer is frequently complicated by pulmonary infections which may impair prognosis of this disease. Therefore, we investigated the effect of bacterial lipopolysaccharides (LPS, Endotoxin) on tumor proliferation in vitro in the non-small cell lung cancer (NSCLC) cell line A549, ex vivo in a tissue culture model using human NSCLC specimens and in vivo in the A549 adenocarcinoma mouse model. LPS induced a time- and dose-dependent increase in proliferation of A549 cells as quantified by MTS activity and cell counting. In parallel, an increased expression of the proliferation marker Ki-67 and cyclooxygenase (COX)-2 was detected both in A549 cells and in ex vivo human NSCLC tissue. Large amounts of COX-2-derived prostaglandin (PG)E2 were secreted from LPS-stimulated A549 cells. Pharmacological interventions revealed that the proliferative effect of LPS was dependent on CD14 and Toll-like receptor (TLR)4. Moreover, blocking of the epidermal growth factor receptor (EGFR) also decreased LPS-induced proliferation of A549 cells. Inhibition of COX-2 activity in A549 cells severely attenuated both PGE2 release and proliferation in response to LPS. Synthesis of PGE2 was also reduced by inhibiting CD14, TLR4 and EGFR in A549 cells. The proliferative effect of LPS on A549 cells could be reproduced in the A549 adenocarcinoma mouse model with enhancement of tumor growth and Ki-67 expression in implanted tumors. In summary, LPS (Endotoxin) induces proliferation of NSCLC cells in vitro, ex vivo in human NSCLC specimen and in vivo in a mouse model of NSCLC. Pulmonary infection may thus directly induce tumor progression in NSCLC.
A 2020 paper investigated initiation of NSCLC by Endotoxin.5
Infection and inflammation serve an important role in tumor development. Toll‑like receptor 4 (TLR4) is a pivotal component of the innate and adaptive immune response during infection and inflammation. Programmed‑death ligand 1 (PD‑L1) is hypothesized as an important factor for non‑small cell lung cancer (NSCLC) immune escape. In the present study, the relationship between TLR4 and PD‑L1, in addition to the associated molecular mechanism, were investigated. TLR4 and PD‑L1 expression in lung cancer tissues were detected using immunohistochemistry, whilst overall patient survival was measured using the Kaplan‑Meier method. The A549 cell line stimulated using lipopolysaccharide (LPS) was applied as the in vitro inflammatory NSCLC model. Associated factors were investigated using reverse transcription‑quantitative PCR and western blotting. Lung cancer tissues exhibited increased PD‑L1 and TLR4 levels compared with those of adjacent para‑cancerous tissues, where there was a positive correlation between TLR4 and PD‑L1 expression. In addition, increased expression of these two proteins was found to be linked with poorer prognoses. Following the stimulation of A549 cells with LPS (Endotoxin), TLR4 and PD‑L1 expression levels were revealed to be upregulated in a dose‑dependent manner, where the ERK and PI3K/AKT signaling pathways were found to be activated. Interestingly, in the presence of inhibitors of these two pathways aforementioned, upregulation of PD‑L1 expression was only inhibited by the MEK inhibitor PD98059, which can inhibit ERK activity. These data suggested that the ERK signaling pathway is necessary for the TLR4/PD‑L1 axis. In conclusion, data from the present study suggest that TLR4 and PD‑L1 expression can serve as important prognostic factors for NSCLC, where TLR4 activation may induce PD‑L1 expression through the ERK signaling pathway.
Smoker and Non-Smoker NSCLC
As previously reported smokers and those breathing other peoples smoke suffer Endotoxin poisoning, so that Jab induced NSCLC might be underestimated.6
I will expand later.
https://www.clinicaltrialsregister.eu/ctr-search/trial/2021-001290-23/results#subjectDispositionSection
Clinical Reviewers: Susan Wollersheim, MD and Ann Schwartz, MD. 23 August 2021. BLA Clinical Review Memorandum.
Katja Hattar, Rajkumar Savai, Florentine S B Subtil, Jochen Wilhelm, Anja Schmall, Dagmar S Lang, Torsten Goldmann, Bastian Eul, Gabriele Dahlem, Ludger Fink, Ralph-Theo Schermuly, Gamal-Andre Banat, Ulf Sibelius, Friedrich Grimminger, Ekkehard Vollmer, Werner Seeger, Ulrich Grandel. 2012. Endotoxin induces proliferation of NSCLC in vitro and in vivo: role of COX-2 and EGFR activation. https://www.spandidos-publications.com/10.3892/ijo.2020.5068
Xiuhua Kang, Penghui Li, Chuibin Zhang, Yunshan Zhao, Huoli Hu, Guilan Wen. 2020. The TLR4/ERK/PD‑L1 axis may contribute to NSCLC initiation.